Introduction
Patients with sickle cell disease (SCD) are at increased risk of perioperative complications following general anesthesia including acute chest syndrome (ACS), vaso-occlusive pain episodes (VOE), and infection. The 2013 Transfusion Alternatives Preoperatively in SCD (TAPS) study found preoperative transfusion of patients with SCD, type SS or SB 0 thalassemia, prior to low- or medium-risk surgeries was associated with decreased perioperative complications. The American Society of Hematology 2020 guidelines for transfusion support for SCD suggest preoperative transfusion for those requiring general anesthesia (GA) lasting > 1 hour; however, it was noted that this should be individualized based on factors such as risk of surgery, baseline hemoglobin (Hb), and disease severity. With more broad use of Hydroxyurea (HU) that improves baseline Hb and decreases ACS and VOE frequency, we lack equipoise for when pre-anesthesia transfusion is indicated. We performed a chart review on pediatric patients with SCD at a large SCD center to determine clinician practice of pre-anesthesia transfusion versus no transfusion for patients on HU and the incidence of post-anesthesia complications with and without pre-anesthesia transfusion.
Methods
We performed an institutional review board approved retrospective chart review of patients with SCD (all genotypes) aged 0 to 22 years who underwent procedures or imaging studies with GA between the years 2019 and 2022 at our institution. Surgical risk score was assigned to all procedures per the TAPS study criteria. We examined the incidence of post-anesthesia complications occurring in the emergency department or hospital within 30 days post-anesthesia. Complications such as VOE, ACS, transfusion-related effects, and infection were recorded as categorical variables.
Results
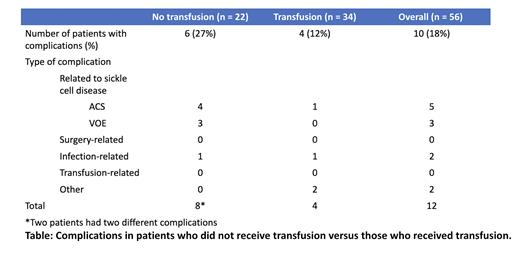
We identified 165 patients with SCD who underwent GA at our center between 2019 and 2022: 56 of these patients were on hydroxyurea and 41 were not on hydroxyurea. We excluded 52 patients on chronic transfusion and 16 who had not consented for participation or had anesthesia encounters during a stem cell transplant admission. Among the 56 patients on HU, 34 received pre-anesthesia transfusion (2 by exchange transfusion) and 22 did not. The average Hb of those on HU who received pre-anesthesia transfusion was 8.64 g/dl (SD 1.1 g/dl) and of those who did not receive transfusion it was 9.4 g/dl (SD 1.33 g/dl) (p = 0.03, unpaired t-test). Among patients on HU who received transfusion, 4/34 (12%) had post-anesthesia complications and of those who did not receive transfusion, 6/22 (27%) had complications (p = 0.17, Fisher exact test) (Table). Among the transfused cohort, complications occurred after 2 low-risk procedures (ACS after an electrophysiology study with radiofrequency ablation and streptococcal infection after an abdominal exploratory laparoscopy), 1 medium-risk procedure (hematuria/abdominal pain after laparoscopic cholecystectomy) and 1 high-risk procedure (respiratory failure after coarctation of the aorta repair). Among patients who were not transfused, complications occurred after 2 imaging studies (ACS in the setting of parainfluenza infection after brain MRI and VOE after shoulder MRI), 2 low-risk procedures (ACS after laparoscopic appendectomy and VOE after adenoidectomy), and 2 medium-risk procedures (ACS after laparoscopic cholecystectomy and multiple admissions for 1 patient for ACS and VOE after endoscopic retrograde cholangiopancreatography).
Conclusions
In patients with SCD -SS or -SB 0 thalassemia on hydroxyurea undergoing procedures with anesthesia at our center, clinicians continued to prescribe pre-anesthesia transfusion for those with a Hb < 9 g/dl. The incidence of complications was higher in patients on HU who did not receive pre-anesthesia transfusion despite an average pre-procedure Hb of > 9 g/dL, but this was not statistically significant in our small sample size. However, these numbers are comparable to the findings of the TAPS study which found that 5/33 (15%) patients in the preoperative transfusion group had clinically important complications compared with 13/33 (39%) patients in the no transfusion group. These findings suggest that despite higher baseline Hb levels in the setting of HU use, patients with sickle cell disease may continue to benefit from pre-anesthesia transfusion but a randomized controlled trial is necessary.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal